In the 1950s, plastics and their requisite chemicals were hailed as miraculous emblems of progress for their role in modernising everyday life. However, we have gradually begun to recognise the consequences of ubiquitous chemical exposures on human health and the ecosystems we depend upon.
After tragedies like the thalidomide scandal and the Bhopal chemical disaster brought awareness to the links between chemicals and chronic health issues, birth defects and cancer, among other afflictions, concern about chemical dangers went mainstream. This spurred legislation like the 1976 US Toxic Substances Control Act (TOSCA), which intended to prevent disease by requiring toxicity testing of new chemicals before market entry as well as existing high-risk chemicals. Yet industry pushback quickly undermined its effectiveness.
Within a year, the US Environmental Protection Agency grandfathered in around 62,000 chemicals already on the market as ‘safe’. “There was a certain momentum built into the chemical industry, where the government looked favourably upon it, didn’t want to criticise it and continued to support it for a long time,” says Dr Phil Landrigan, professor of biology and director of the Global Public Health Program and Global Observatory on Planetary Health at Boston College. Only five chemicals have been removed under TOSCA, despite tens of thousands more entering markets, setting a tone of lax regulation that persists today despite mounting evidence of hazards.
European regulation is similarly constrained. The EU’s chemical legislation, known as REACH, aims to register and restrict substances of very high concern, including those that are carcinogenic, mutagenic and reprotoxic and those that are persistent, bioaccumulative and toxic. “On paper, REACH is a lot stronger than TOSCA, but in practice, it’s not a whole lot different,” says Dr Landrigan. “It has been a bit more effective at getting chemicals off the market, but it still relies very heavily, for example, on testing undertaken by the industries themselves, which creates an inherent conflict of interest.”
As a result of lags in regulation, there are many chemicals in use with unknown health impacts. The number of chemicals in plastics is now estimated to be around 16,000, most of which have never been tested for toxicity, meaning that we have not measured their true cost. We know that two million lives were lost to exposure to selected chemicals in 2021. However, data are only available for a certain number of chemicals due to gaps in scientific evidence, so, in reality, these numbers could be far higher.

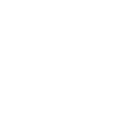
A contaminated ocean
Many chemical exposures occur through waterways, as industrial and agricultural runoff carries chemicals into surface waters, groundwater supplies and water treatment facilities, as well as soil and farmland. Fossil fuel operations are a key source of water contamination. There are 1,021 chemicals, some of them suspected carcinogens, in the fluids and wastewater resulting from fracking alone. An evaluation of these chemicals for potential reproductive and developmental toxicity found that data were available for only 24% of these chemicals, 65% of which presented potential adverse reproductive and developmental effects.
Another category of chemicals that are ubiquitous in waterways is PFAS (per- and polyfluoroalkyl substances), known as “forever chemicals”. Over 2,000 of these chemicals are present in drinking water, streams and ocean ecosystems, with at least 45% of tap water across the US believed to be contaminated. These chemicals have been associated with a wide range of adverse health effects, including impairments to the immune, endocrine, developmental, reproductive and neurological systems, as well as elevated risks of various cancers. It is now estimated that a large percentage of people carry detectable levels of PFAS in their bloodstream.
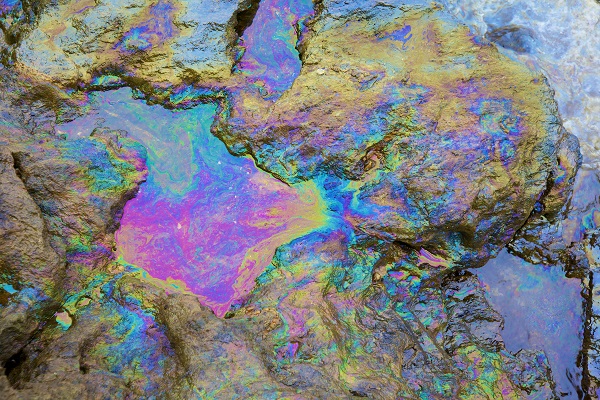
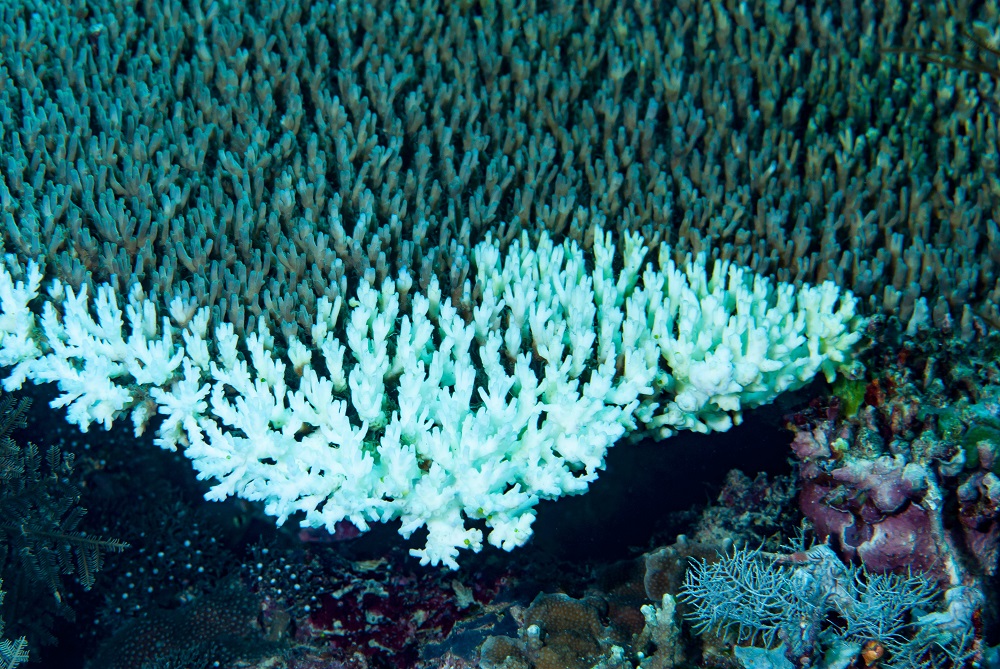
Contaminated water is not the only health threat posed by ocean pollution. Chemical runoff from agricultural and industrial activities disrupts marine nutrient balances, fuelling excessive algal blooms that deplete oxygen levels in the ocean and produce biotoxins. Algal toxins like ciguatera and domoic acid accumulate in fish and shellfish, which can then cause severe neurological effects, including dementia, paralysis and even death, if consumed by humans.
Moreover, there is mounting evidence that coastal pollution enables the proliferation of harmful bacteria such as vibrio, which can infect people with life-threatening illnesses like cholera. By creating hypoxic dead zones and concentrating biotoxins in the food chain, chemical contamination transforms once-thriving marine ecosystems into vectors for human disease on a global scale.
The plastic connection
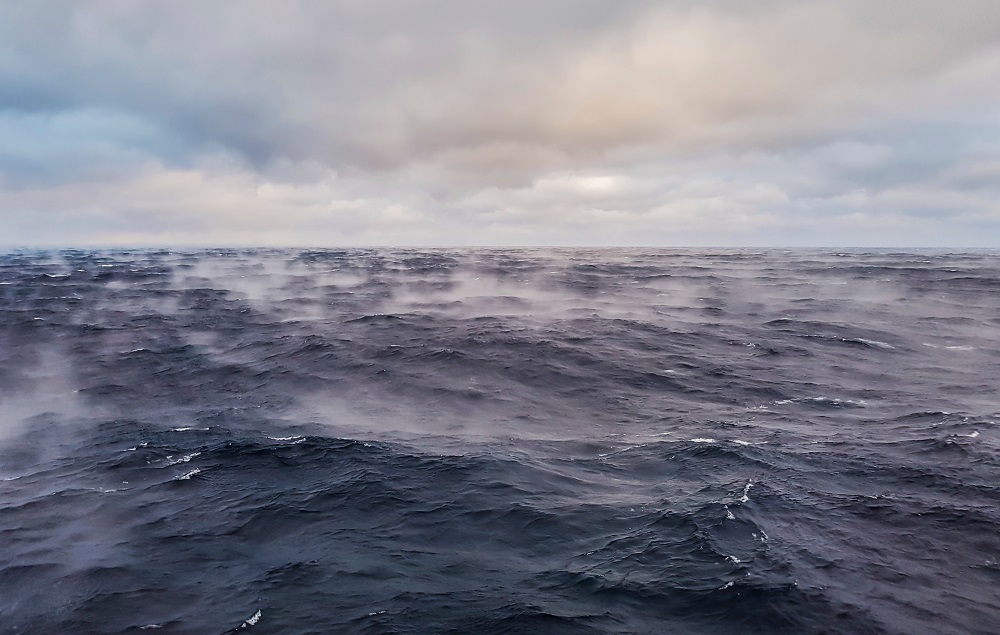
Plastics are a major pathway for chemicals entering oceans. Thousands of chemicals are used during manufacturing to create various polymer types and provide specific properties like colour, flexibility or fire resistance. Additional chemicals can inadvertently be incorporated or released from plastics during their use and breakdown. Residents of communities adjacent to plastic production and waste disposal sites experience increased risks of premature birth, low birth weight, asthma, childhood leukaemia, cardiovascular disease, chronic obstructive pulmonary disease and lung cancer.
Of the more than ten million tonnes of plastic entering the oceans yearly, most will fragment into microplastics—tiny particles that soak up and transport chemicals along with them. These microplastic particles then accumulate in drinking water sources and seafood, leading to human ingestion of millions of particles laden with chemicals. This cycle results in plastics acting as vectors that constantly introduce chemicals into marine environments and subsequently into humans.
“Once plastic is out, it’s out, and it’s going to stay in the environment for a long time—including all the chemicals in the plastic,” says Dr Landrigan. “The only way to slow down exposure to these chemicals is to slow it down through global production caps. Chemical and plastic production are on track to double by 2040, and that’s just not sustainable.”

Shifting the regulatory landscape
International efforts, such as a proposed global plastic treaty, aim to tackle this focus, with a particular focus on regulating the chemicals in plastic. National chemical regulations are also increasingly recognising the role of plastics in addressing the scourge of chemical pollution.
The EU’s chemicals restriction roadmap aims to extend REACH to include PFAS, bisphenols and flame retardants. However, progress on implementing the roadmap has been sluggish. In 2023 the EU did enact new REACH rules prohibiting intentionally added microplastics, covering all synthetic polymer particles below five millimetres that are organic, insoluble and resist degradation. Still, it remains nearly impossible to prevent plastics in the environment from fragmenting into microplastics without drastic cuts to overall plastic production.
Establishing explicit links between chemical exposures and health impacts has historically challenged policymakers as industries push back against efforts to ban their products without overwhelming evidence. Fortunately, advancements in biomonitoring have enabled blood and urine screenings to test for hundreds of chemicals. Moreover, findings like the recent discovery of a correlation between microplastics in arteries and cardiovascular disease, stroke and death underscore how ubiquitous plastic exposure has become.
Another key advancement is in public health studies. According to Dr Landrigan, the benefits of prospective epidemiologic studies are increasingly recognised—these studies enrol women during pregnancy and then follow their babies over many years as they go through childhood, which helps gain a more comprehensive understanding of what chemicals they are exposed to and what illnesses they may face. The results of these studies are powerful tools for establishing causation. “We’re in a much better position today to establish links between chemicals and disease than we used to be,” says Dr Landrigan. Establishing these links with more certainty will be crucial for crafting more comprehensive policies that capture all harmful chemicals.
Currently, an overwhelming amount of evidence must be available for a chemical to be banned outright. The US is an extreme example, as asbestos was only fully banned this past month, despite decades of evidence that exposure causes cancer and mesothelioma and its ban in over 50 countries. While European legislation is somewhat more comprehensive, it still has significant gaps. The phasing out of PFAS has been slowed by industry pushback, and even the strictest proposed regulations still allow PFAS in functions deemed “essential”.
While accumulating more evidence to justify restricting chemicals is welcome progress, meaningful change will require a more proactive approach. The current approach runs contrary to the precautionary principle, which is paramount in many scientific and public health strategies. Doctors act on credible evidence of risk to protect patients from potential dangers; public health policy follows a similar preventative model, erring on the side of caution when human life is at stake.
Therefore, a more cautious regulatory approach would restrict chemicals once a credible risk is demonstrated, placing the onus on manufacturers to prove an acceptable hazard threshold rather than the other way around. “There needs to be a paradigm shift in national legislation and international treaties that takes away this presumption that chemicals are harmless until proven to cause damage,” says Dr Landrigan.
EXPLORE MORE CONTENT ABOUT THE OCEAN
Back to Blue is an initiative of Economist Impact and The Nippon Foundation
Back to Blue explores evidence-based approaches and solutions to the pressing issues faced by the ocean, to restoring ocean health and promoting sustainability. Sign up to our monthly Back to Blue newsletter to keep updated with the latest news, research and events from Back to Blue and Economist Impact.
The Economist Group is a global organisation and operates a strict privacy policy around the world.
Please see our privacy policy here.
THANK YOU
Thank you for your interest in Back to Blue, please feel free to explore our content.
CONTACT THE BACK TO BLUE TEAM
If you would like to co-design the Back to Blue roadmap or have feedback on content, events, editorial or media-related feedback, please fill out the form below. Thank you.
The Economist Group is a global organisation and operates a strict privacy policy around the world.
Please see our privacy policy here.




 World Ocean Summit & Expo
2025
World Ocean Summit & Expo
2025 UNOC
UNOC Sewage and wastewater pollution 101
Sewage and wastewater pollution 101 Slowing
the chemical tide: safeguarding human and ocean health amid
chemical pollution
Slowing
the chemical tide: safeguarding human and ocean health amid
chemical pollution Hazardous chemicals in plastics - the discussions at INC
Hazardous chemicals in plastics - the discussions at INC